I think “Pregnancy “is one of the most important dreams in your life. Because it is fundamental to a family. However, planning the pregnancy and pre-pregnancy care is the most important.
Some commonly asked questions from me are “What is the average weight gain during pregnancy?” and “What is the recommended weight gain during pregnancy?”. In addition, another common problem is “How to maintain BMI during pregnancy?”. So, today I will discuss the most essential facts on this matter.
Inadequate weight gain during pregnancy is a major cause of pregnancy complications in the developing world. While excess weight gain is a significant risk factor for pregnancy complications in developed countries. Therefore I think it is better to know the good/ optimal weight gain during pregnancy. Unless you would encounter many issues compared to mothers with average weight gain during pregnancy.
A few decades back, when we discussed the adequacy of body build, we discussed “Weight vs. Height”. However, this concept has been replaced by a concept called BMI. It is a better indicator of someone’s body build than height and weight.
In addition, the Institute of Medicine (IOM) has recommended BMI to measure the adequacy of weight gain during pregnancy. Therefore we can’t have a complete discussion on average weight gain during pregnancy without knowing the concept of BMI (Body Mass Index). Because the amount of weight gain during pregnancy should tally with the BMI.
What is Body Mass Index (BMI)?
BMI, or Body mass index, is a parameter of the adequacy of body build. It is a suitable parameter of a healthy lifestyle and the chance of getting a particular illness.
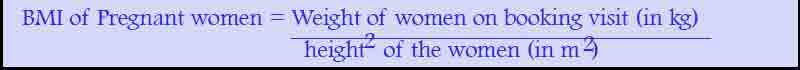
The calculation of BMI is straightforward, and it is known to everyone. You must divide your weight (kg) by the square of height (m2).
According to the results of the BMI calculation, you are categorized as underweight, average weight, overweight, obese I, and Obese II. This BMI range may vary according to the Region.
How to calculate the BMI during Pregnancy?
Pregnancy is a rapid weight-gaining period. You would increase at least some of your weight whenever you are pregnant.
Measuring BMI during pregnancy is a difficult task as it includes the baby’s weight too. Therefore we will take the pregnant lady’s initial weight to calculate BMI. So, the BMI should be recorded in the booking visit. Unless it is challenging to calculate average weight gain during pregnancy for you.
BMI in Pregnancy = Weight at the booking visit(kg)/ Height2 at the booking visit (m2)
Overweight during pregnancy
Who is called an obese mother? Although it is a common term used in the community, you should have a BMI of 30 or more to be categorized as obese. So the BMI in pregnancy should be used to identify these groups.

This group belongs to mothers with both obesity I and II. Most of the time, we have found this group in developed countries or patients with good socio-economic status. They have shown a particular risk for a set of health issues than other mothers.
What are the maternal pregnancy complications for mothers with obesity?
Do you know you are in a high-risk group for some pregnancy-related illnesses? Yes, sometimes you may have faced these problems already. According to recent studies, women with very high BMI are a risk of Diabetes, hypertension, pregnancy-induced hypertension (PIH) and primary cesarean section delivery and a lot more.
1. Gestational Diabetes
Gestational Diabetes is a condition with a marked increase in blood sugar levels during pregnancy. This causes problems for both baby and mother during pregnancy and even after.
A mother with Gestational Diabetes is at risk of developing hyperglycemic events, DKA, frequent urinary infections, etc.
It has also been proven that women with gestational Diabetes are prone to get pre-term babies, macrosomic babies and miscarriages. In addition, it is found that they may have babies with a lot of congenital abnormalities.
2. Hypertension during pregnancy (PIH, Hypertension)
This is the other major pregnancy issue. Pregnant ladies with hypertension are a risk of pre-eclampsia, eclampsia and several other significant life-threatening problems.
- Babies of these women have the risk of placental abruption and PPH.
- Primary Cesarean section
- Mothers with obesity have a risk of macrosomic babies (large babies). As a result, there are several problems during the delivery.
What are the fetal complications in mothers with obesity?
Do you know that if you are obese, you risk your additional baby risk? Although it is hard to believe, it is true. You are adding additional risk to your baby in different ways.
“Obesity increases the risk of macrosomia, pre-term births, stillbirths, Pregnancy losses, congenital disabilities and several more.“
American College of Obstetrics and Gynecologists
1. Macrosomia
Macrosomia is a condition of larger babies than average. Usually, it is common among obese and diabetic mothers. The risk of macrosomia is mainly the risk of birth injuries.
E.g., Bell’s palsy
In addition, both mother and baby have to face the stressful situation at the time of birth. This is more painful and traumatic than delivering an average-sized baby.
2. Miscarriages
This is another complication of obesity. According to the current evidence, obese people have a high chance of early pregnancy loss.
3. Stillbirths
In addition to miscarriages, these mothers also have a high risk of late pregnancy loss. These are called stillbirths.
4. Congenital disabilities
Another common problem is congenital disabilities among obese people. It is found that Neural tube defects and some other congenital abnormalities are more common among the babies of these mothers.
How to prevent complications associated with obesity?
Obesity or uncontrolled high BMI is associated with numerous complications for you and your baby. Therefore it is your responsibility to minimize such complications in your pregnancy. This is a step-by-step guideline on how to minimize pregnancy-associated complications in obesity.
a. Maintain healthy BMI and weight gain
Imagine you are a lady with a BMI of 35 during your typical day-to-day life. Then you get pregnant suddenly. Now you are ended up in mothers with an obese BMI range. So you can’t reverse your BMI to normal BMI after getting pregnant.

Therefore always try to maintain your BMI in day-to-day life. Unless you can’t be in the mothers with healthy weight gain during pregnancy.
b. Take pre-pregnancy folic acid
Obese mothers are at high risk of congenital abnormalities, including Neural Tube Defects. If you are getting recommended amount of folic acid every day, you are in the safe group. Therefore, you must start “pre conceptional folic acid” at least 3 months before getting pregnant.
c. Do not forget pre-pregnancy counselling
Pre-pregnancy counselling has an important role when you are planning to go for a pregnancy. You can get an idea of your risk factors, the necessary steps to prevent them and how to avoid complications during pregnancy.
Although it is a routine procedure for most mothers, there is a lack of pre-pregnancy counselling in some countries. So, you should undergo this pre-pregnancy counselling process. In that case, you can have excellent details about optimal BMI in pregnancy, how to maintain a proper diet plan, what is abnormal or normal weight gain during pregnancy, etc.
d. Optimize your medical conditions
Most of the time, obesity is associated with Diabetes and hypertension. If you are a patient with Diabetes or hypertension, do not forget to get optimized before getting pregnant. Additionally, have a review on your current medications too.
e. Undergo regular medical checkups and ultrasound scan
Every pregnant mother should undergo a regular medical checkup to rule out some pregnancy-related and non-pregnancy-related issues. In your pregnancy clinic, you would have to check Full blood count (FBC), Urine full report (UFR), Blood sugar measurements, etc. The importance of these is for early identification of future risk conditions.
In addition, you need to go for several ultrasound scans. This includes dating scan, anomaly scan and growth scan and etc. In obese ladies, all these ultrasound measurements are essential.
As obesity is associated with a lot of congenital abnormalities, the most critical scan would be an anomaly scan. This would be performed around 20 weeks. Here you can early identify and optimize some anomalies. Neural tube defects are some of the common anomalies in pregnancy. Another important ultrasound scan is a growth scan. In some settings, you would have to face a series of growth scans to exclude growth problems. You have to have a proper scan to rule out macrosomia in pregnancy.
f. Have a nutritious diet
Diet is one of the significant factors associated with obesity. You will not have a high BMI if you have reasonable control over your diet. Then it is easy to have a healthy weight gain during a pregnancy instead of having troublesome weight gain. It is always necessary to avoid the unnecessary amount of dietary sugar and fat.
Is it okay to have diet control during pregnancy?
When we discuss reducing the sugar content, you might imagine whether it is okay to have diet control during pregnancy. No, absolutely not. It would help if you did not try to reduce your weight during pregnancy to avoid pregnancy complications. It is far more problematic than being obese.
However, you can still try to minimize unnecessary sugar during pregnancy. Also, you can add a lot of nutritious foods like vegetables, fruits, etc. Then only you can have precise control over your diet.
Low weight during pregnancy
What is low BMI or low weight during pregnancy? Here, IOM defines less than 18.5 as a low BMI. If you are below the level of 18.5, it is advisable to improve some weight before getting pregnant. Because an adequate amount of weight gain during pregnancy is significant for the well-being of antenatal and post-natal periods. Like obesity and overweight among pregnant mothers in countries like the UK, the US and etc., Low BMI/ underweight among mothers has become a problem in countries with low economic capacity. Surprisingly new research has shown that it is a widespread problem in Japan too.
Being underweight during pregnancy causes several issues for the baby during and after pregnancy. For example, it causes pre-term deliveries, small for gestation and low birth weight. Some modern studies have shown that low BMI during pregnancy also causes problems in intellectual development in childhood.
Recommended optimal/ average weight gain during pregnancy
As we mentioned earlier, “The Institute Of Medicine (IOM)” recommends BMI as a primary indicator of measuring the adequacy of weight during pregnancy. According to the pregnancy weight gain guidelines of the Institute of medicine, you have to gain more if you are low, and you have to gain a minimum of weight if you are obese.
These are the current recommendation for maintain average weight gain during pregnancy.
• Underweight (< 18.5 kg/m2); total weight gain range: 28 to 40 pounds (12.5 – 18 kg)
• Normal weight (18.5 – 24.9 kg/m2); total weight gain range: 25 to 35 pounds (11.5 – 16 kg)
• Overweight (25.0 – 29.9 kg/m2); total weight gain range: 15 to 25 pounds (7 – 11.5 kg)
• Obese (≥ 30.0 kg/m2); total weight gain range: 11 to 20 pounds (5 – 9 kg)
Importance of optimal weight gain during pregnancy
According to some of the newel research, most women of pregnancy age are out of the optimal level of BMI before pregnancy. This will cause a lot of additional risk for the baby and you. As we have already discussed, both the underweight and the obesity is giving additional risks.
Now you know the importance of maintaining a healthy BMI before and during pregnancy. Therefore, it is time to discuss the optimal weight gain during pregnancy.
According to the current recommendation by the National Institute of Medicine, underweight women should gain more weight while obese women gain less weight. However, it is found that the risk caused by more weight gain is high in underweight mothers.
Therefore if you gain the optimal level of weight, your baby will be inadequate in size and weight. Also, you would get a minimum of complications during and after the delivery. Therefore it is essential to maintain an average weight gain during pregnancy.
How to maintain adequate weight before and during pregnancy
As we have discussed, there is a large percentage of mothers with either high BMI or low BMI. Therefore it is essential to optimize the BMI before and during the pregnancy. This will reduce the problems associated with high or low BMI. As it is not advisable to reduce or increase weight in large proportions, you must follow the essential health tips to have a good BMI.
A step-by-step guide to maintaining average weight gain during pregnancy
Step 1 – Have a BMI assessment on and off.
Measurement of weight and height is not hard in the day to day life. If you can measure them, the calculation of BMI is straightforward. If possible, have an idea of your monthly BMI. Then you can maintain a normal BMI before pregnancy and have an average weight gain during pregnancy.
Step 2 – Follow healthy but nutritious food habits
Food is the main factor for your BMI, body build or weight. Unless you eat a healthy and balanced diet, you have to face many difficulties maintaining a healthy BMI. Because unnecessary dietary energy intake will make you obese and unhealthy. Conversely, if you do not take adequate energy in your diet, you will be thin too.
So the best option is to maintain a nutritious and balanced diet. Then you can initiate the process of healthy weight gain during pregnancy. Even during antenatal, you can continue this healthy diet plan with simple alterations. You can have some help for your dietitian for this alteration. So if you try to maintain good dietary habits, you can gain average weight during pregnancy.
Step 3: Have regular exercise.
Regular exercise is the most common approach to reducing obesity. Even if you are not obese, you can use these methods to maintain an average weight. This is crucial in reducing stress, increasing muscle strength and reducing future health hazards.
Is it safe to exercise during pregnancy? This is a common question during antenatal visits. You can’t do stressful exercises like weight-bearing and other anaerobic exercises. But still, you can have some light exercise. This will help to maintain your weight within the optimal level for the pregnancy. Therefore, exercise is fundamental to maintaining average weight gain during pregnancy.
Step 4 – Have stress free lifestyle.
Mental health is an essential component of day-to-day activities.
Step 5: Avoid alcohol consumption.
Alcohol causes a lot of problems for your baby. In addition, it may alter the pattern of weight gain during pregnancy. Therefore it is essential to avoid alcohol during pregnancy.
Never use alcohol during pregnancy – Serious side effects of alcohol consumption in pregnancy

